- >>
- Disease Studies
- BANDA: Connectomes Related to Anxiety & Depression
- Study Homepage
Study Overview
The Connectomes Related to Anxiety and Depression in Adolescents Project, also known as Boston Adolescent Neuroimaging of Depression and Anxiety (BANDA) is a collaborative effort among researchers at the Massachusetts General Hospital (MGH), Massachusetts Institute of Technology (MIT), McLean Hospital, and Boston University. We will focus on understanding psychiatric disorders in adolescence, in particular those associated with two leading causes of death in adolescents and young adults (suicide and substance-abuse related accidents). Our research is guided by the “Acute Threat/Fear” and the “Reward/Prediction Error” construct.
Project Timespan: Sept. 16, 2015 - June 20, 2019
Investigators
Study Protocol Overview
Data being collected
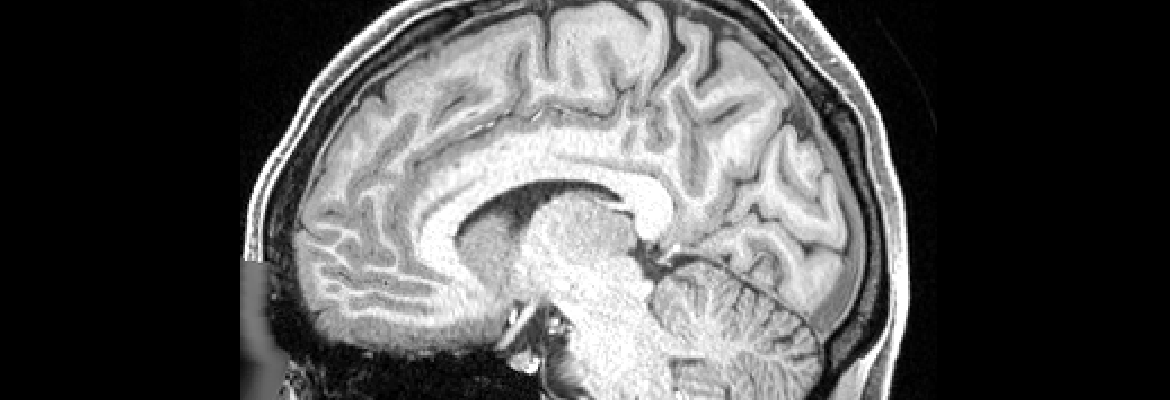
All imaging will be conducted at Massachusetts General Hospital on one of three scanners: A 3T Siemens Prisma, 3T Siemens ConnectomA, and 7T Siemens. A limited version of the HCP Lifespan scanning protocol will be implemented with the intent of keeping the total MR scanning time to under 2 hours.
- Standard HCP demographics.
- Imaging: The imaging modalities are structural, diffusion, and functional (both resting state and task) with the following tasks: emotion processing, incentive processing, social cognition, working memory/category-specific representations.
- Clinical: Child Schedule for Affective Disorders and Schizophrenia Present and Lifetime Version, Revised Child Anxiety and Depression Scale, Beck Depression Inventory-II, Snaith-Hamilton Pleasure Scale, State-Trait Anxiety Inventory, Behavioral Inhibition System and Behavioral Activation System Questionnaire, Beck Scale for Suicidal Ideation, Risky Behavior Questionnaire for Adolescents, Stress and Adversity Inventory.
- Behavioral: NIH toolbox, HCP behavioral measures, fear learning and extinction, biased attention to threat.
Cohort Description
The study includes of 225 adolescents ages 14-17. Of these, 45 are healthy controls, and 180 are participants with and without anxiety and/or depression.
Data Release Plans
- The first data release includes 75 participants.
- The second data release includes 150 participants.
- The third data release includes 225 participants.
Keywords:
Adolescent; Anxiety; Mental Depression; Mood Disorders; White Matter
For More Information:
Boston Adolescent Neuroimaging of Depression and Anxiety (BANDA)
Current Data Releases
BANDA Release 1.1 Released on 03/04/2024
The updated BANDA Release 1.1 of imaging and behavioral data is now available in the NIMH Data Archive (NDA, DOI: 10.15154/3tk5-pb47). The Boston Adolescent Neuroimaging of Depression and Anxiety (BANDA) is a study of 215 adolescents ages 14-17, 152 of whom had a current diagnosis of a DSM-5 (APA, 2013) anxious and/or depressive disorder. The BANDA study collected a rich dataset of brain, clinical, and cognitive/neuropsychological measures from these adolescent subjects.
BANDA Release 1.1 on NDA contains changes to non-MRI data from the BANDA 1.0 Release. Corrections were made to some elements and/or new composite/summary elements were added to several NDA structures (see change log in documentation). Note: To assure reproducibility, any non-MRI data accessed from the BANDA 1.0 release should be replaced entirely by those of the BANDA 1.1.
BANDA Release 1.1 data includes:
- unprocessed data of all modalities (structural MRI, resting state fMRI, task fMRI for 3 tasks, and diffusion MRI) for up to 207 subjects
- minimally preprocessed MRI data of all modalities for up to 203 subjects
- updated clinical and behavioral data for 215 subjects: updates include addition of composite/summary scores for many and corrections for 3 NDA structures
Get Access and Download the data: Get started with the Data Access and Download Instructions for obtaining access, navigating NDA and using its download tools. We've also created a wiki that details setup steps for downloading data via NDA's command line tools.
The released data are available on NDA as:
- BANDA11Rec package of recommended preprocessed + behavioral data (497 GB, OPTION ONE)
- BANDA11AllFiles package (5.9 TB, OPTION ONE)
- BANDA11ImgManifestBeh package of imaging manifests + behavioral data (245 MB, OPTION ONE)
- or can be filtered on by modality and processing level to create a custom package of a subset of the data (OPTION TWO).
Want more information? Check out our documentation to help with understanding the project and interpreting the data.
View Data Release Documentation
Release Date: Mar 04, 2024
Publications
-
Brain function and clinical characterization in the Boston adolescent neuroimaging of depression and anxiety study.
Show SummaryWe present a Human Connectome Project study tailored toward adolescent anxiety and depression. This study is one of the first studies of the Connectomes Related to Human Diseases initiative and is collecting structural, functional, and diffusion-weighted brain imaging data from up to 225 adolescents (ages 14-17 years), 150 of whom are expected to have a current diagnosis of an anxiety and/or depressive disorder. Comprehensive clinical and neuropsychological evaluations and longitudinal clinical data are also being collected. This article provides an overview of task functional magnetic resonance imaging (fMRI) protocols and preliminary findings (N = 140), as well as clinical and neuropsychological characterization of adolescents. Data collection is ongoing for an additional 85 adolescents, most of whom are expected to have a diagnosis of an anxiety and/or depressive disorder. Data from the first 140 adolescents are projected for public release through the National Institutes of Health Data Archive (NDA) with the timing of this manuscript. All other data will be made publicly-available through the NDA at regularly scheduled intervals. This article is intended to serve as an introduction to this project as well as a reference for those seeking to clinical, neurocognitive, and task fMRI data from this public resource.
-
Image acquisition and quality assurance in the Boston Adolescent Neuroimaging of Depression and Anxiety study.
Show SummaryThe Connectomes Related to Human Diseases (CRHD) initiative was developed with the Human Connectome Project (HCP) to provide high-resolution, open-access, multi-modal MRI data to better understand the neural correlates of human disease. Here, we present an introduction to a CRHD project, the Boston Adolescent Neuroimaging of Depression and Anxiety (BANDA) study, which is collecting multimodal neuroimaging, clinical, and neuropsychological data from 225 adolescents (ages 14-17), 150 of whom are expected to have a diagnosis of depression and/or anxiety. Our transdiagnostic recruitment approach samples the full spectrum of depressed/anxious symptoms and their comorbidity, consistent with NIMH Research Domain Criteria (RDoC). We focused on an age range that is critical for brain development and for the onset of mental illness. This project sought to harmonize imaging sequences, hardware, and functional tasks with other HCP studies, although some changes were made to canonical HCP methods to accommodate our study population and questions. We present a thorough overview of our imaging sequences, hardware, and scanning protocol. We detail similarities and differences between this study and other HCP studies. We evaluate structural-, diffusion-, and functional-image-quality measures that may be influenced by clinical factors (e.g., disorder, symptomatology). Signal-to-noise and motion estimates from the first 140 adolescents suggest minimal influence of clinical factors on image quality. We anticipate enrollment of an additional 85 participants, most of whom are expected to have a diagnosis of anxiety and/or depression. Clinical and neuropsychological data from the first 140 participants are currently freely available through the National Institute of Mental Health Data Archive (NDA).
-
Predictive analytics in mental health: applications, guidelines, challenges and perspectives.
Show SummaryThe emerging field of 'predictive analytics in mental health' has recently generated tremendous interest with the bold promise to revolutionize clinical practice in psychiatry paralleling similar developments in personalized and precision medicine. Here, we provide an overview of the key questions and challenges in the field, aiming to (1) propose general guidelines for predictive analytics projects in psychiatry, (2) provide a conceptual introduction to core aspects of predictive modeling technology, and (3) foster a broad and informed discussion involving all stakeholders including researchers, clinicians, patients, funding bodies and policymakers.
-
Altered Intrinsic Functional Brain Architecture in Children at Familial Risk of Major Depression.
Show SummaryNeuroimaging studies of patients with major depression have revealed abnormal intrinsic functional connectivity measured during the resting state in multiple distributed networks. However, it is unclear whether these findings reflect the state of major depression or reflect trait neurobiological underpinnings of risk for major depression.
-
Brain connectomics predict response to treatment in social anxiety disorder.
Show SummaryWe asked whether brain connectomics can predict response to treatment for a neuropsychiatric disorder better than conventional clinical measures. Pre-treatment resting-state brain functional connectivity and diffusion-weighted structural connectivity were measured in 38 patients with social anxiety disorder (SAD) to predict subsequent treatment response to cognitive behavioral therapy (CBT). We used a priori bilateral anatomical amygdala seed-driven resting connectivity and probabilistic tractography of the right inferior longitudinal fasciculus together with a data-driven multivoxel pattern analysis of whole-brain resting-state connectivity before treatment to predict improvement in social anxiety after CBT. Each connectomic measure improved the prediction of individuals' treatment outcomes significantly better than a clinical measure of initial severity, and combining the multimodal connectomics yielded a fivefold improvement in predicting treatment response. Generalization of the findings was supported by leave-one-out cross-validation. After dividing patients into better or worse responders, logistic regression of connectomic predictors and initial severity combined with leave-one-out cross-validation yielded a categorical prediction of clinical improvement with 81% accuracy, 84% sensitivity and 78% specificity. Connectomics of the human brain, measured by widely available imaging methods, may provide brain-based biomarkers (neuromarkers) supporting precision medicine that better guide patients with neuropsychiatric diseases to optimal available treatments, and thus translate basic neuroimaging into medical practice.
-
Functional and structural brain correlates of risk for major depression in children with familial depression.
Show SummaryDespite growing evidence for atypical amygdala function and structure in major depression, it remains uncertain as to whether these brain differences reflect the clinical state of depression or neurobiological traits that predispose individuals to major depression. We examined function and structure of the amygdala and associated areas in a group of unaffected children of depressed parents (at-risk group) and a group of children of parents without a history of major depression (control group). Compared to the control group, the at-risk group showed increased activation to fearful relative to neutral facial expressions in the amygdala and multiple cortical regions, and decreased activation to happy relative to neutral facial expressions in the anterior cingulate cortex and supramarginal gyrus. At-risk children also exhibited reduced amygdala volume. The extensive hyperactivation to negative facial expressions and hypoactivation to positive facial expressions in at-risk children are consistent with behavioral evidence that risk for major depression involves a bias to attend to negative information. These functional and structural brain differences between at-risk children and controls suggest that there are trait neurobiological underpinnings of risk for major depression.
-
Prediction as a humanitarian and pragmatic contribution from human cognitive neuroscience.
Show SummaryNeuroimaging has greatly enhanced the cognitive neuroscience understanding of the human brain and its variation across individuals (neurodiversity) in both health and disease. Such progress has not yet, however, propelled changes in educational or medical practices that improve people's lives. We review neuroimaging findings in which initial brain measures (neuromarkers) are correlated with or predict future education, learning, and performance in children and adults; criminality; health-related behaviors; and responses to pharmacological or behavioral treatments. Neuromarkers often provide better predictions (neuroprognosis), alone or in combination with other measures, than traditional behavioral measures. With further advances in study designs and analyses, neuromarkers may offer opportunities to personalize educational and clinical practices that lead to better outcomes for people.
-
Selective development of anticorrelated networks in the intrinsic functional organization of the human brain.
Show SummaryWe examined the normal development of intrinsic functional connectivity of the default network (brain regions typically deactivated for attention-demanding tasks) as measured by resting-state fMRI in children, adolescents, and young adults ages 8-24 years. We investigated both positive and negative correlations and employed analysis methods that allowed for valid interpretation of negative correlations and that also minimized the influence of motion artifacts that are often confounds in developmental neuroimaging. As age increased, there were robust developmental increases in negative correlations, including those between medial pFC (MPFC) and dorsolateral pFC (DLPFC) and between lateral parietal cortices and brain regions associated with the dorsal attention network. Between multiple regions, these correlations reversed from being positive in children to negative in adults. Age-related changes in positive correlations within the default network were below statistical threshold after controlling for motion. Given evidence in adults that greater negative correlation between MPFC and DLPFC is associated with superior cognitive performance, the development of an intrinsic anticorrelation between MPFC and DLPFC may be a marker of the large growth of working memory and executive functions that occurs from childhood to young adulthood.
-
Predicting treatment response in social anxiety disorder from functional magnetic resonance imaging.
Show SummaryCurrent behavioral measures poorly predict treatment outcome in social anxiety disorder (SAD). To our knowledge, this is the first study to examine neuroimaging-based treatment prediction in SAD.
Data Use Terms
When users request access to the NIMH Data Archive (NDA), they sign the NDA Data Use Certification (DUC) under which the data is shared. This DUC is usually submitted to the NDA electronically, but this printable version can also be submitted to NDAhelp@mail.nih.gov.
More information on obtaining NDA access is available in the Data Access and Download Instructions.