Study Overview
The goal of this project is to identify connectome-specific correlates and predictors of successful treatment outcome in patients with severe depression followed prospectively while receiving one of three rapidly acting therapeutic interventions. These interventions include electroconvulsive therapy (ECT), serial ketamine infusion and total sleep deprivation (TSD). Via neurostimulation, pharmacological or behavioral perturbation, each elicits relatively robust antidepressant effects and has a distinct mode of access to the central nervous system. A related goal is to characterize variations in neural connectivity associated with individual clinical, behavioral or physiological factors that distinguish patients with severe depression from demographically similar non-depressed controls. Since response to standard antidepressant therapies is moderate, variable, and protracted, understanding how brain networks change with rapid clinical improvement could provide a key opportunity to devise more immediate, personalized and effective treatment and prevention strategies for refractory depression.
Project Timespan: Sept. 2, 2016 - May 31, 2020
Investigators
Study Protocol Overview
Data Being Collected
- Standard HCP demographics
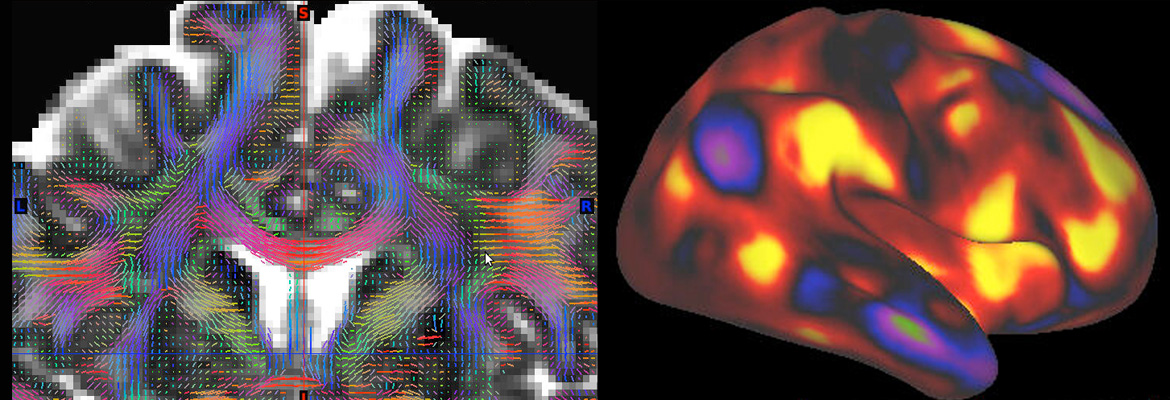
- Imaging: Structural, functional (resting state and task), diffusion and perfusion MRI data collected on Siemens 3T Prisma system located at UCLA is acquired using sequences identical to those developed for the HCP-Aging Project. Functional imaging tasks probe emotional processing and cognitive control.
- Clinical Assessments (Baseline): Structured Clinical Interview for DSM-5, Research Version (SCID-5-RV); Antidepressant Treatment History Form (ATHF); Prescribed Medication History Questionnaire; ChronoType Questionnaire; PhenX Toolkit Substance Abuse and Addiction Questionnaires; Fagestrom Test for Nicotine Dependence; Daily Stress Inventory; Stress and Adversity Inventory (STRAIN); Parental Bonding and Early Life Events Questionnaire; Behavioral Inhibition and Activation System Questionnaires (BIS/BAS), Migraine Screener; World Health Organization Disability Assessment Schedule (WHODAS); National Network of Depression Centers Comorbidity Questionnaire; Combined Trait Rumination Questionnaire.
- Clinical Assessments (Repeated): Hamilton Depression Rating Scale, 17 item (HAMD-17); Inventory of Depressive Symptomatology – Clinician Rated (IDS-C); Computerized Adaptive Tests for Depression, Anxiety, Mania/Hypomania, and Suicide (CAT-MH); Young Mania Rating Scale (YMRS); Quick Inventory of Depressive Symptomatology – Self-Rated (QIDS-SR); Depression Anxiety Stress Scales (DASS); Combined State Rumination Questionnaire; Snaith-Hamilton Pleasure Scale (SHAPS); Apathy Evaluation Scale (AES); Pittsburg Sleep Quality Index; Patient-Reported Outcomes Measurement Information System (PROMIS) Anxiety Test.
- Behavioral Assessments: NIH Toolbox and University of Pennsylvania Computerized Neuropsychological (PennCNP) Tests; Autobiographical Memory Test, Effort Expenditure for Rewards Task.
- Repeated Physiological Measures: Plasma for gene expression analyses and storage of DNA for future genotyping.
Cohort Description
Subjects include 200 patients with severe depression clinically eligible to receive ECT (n=60), serial ketamine (n=60) or TSD (n=80) and 140 controls, combining control data collected locally (n=40) with data from the HCP resource (n=100). Each patient will receive MRI, behavioral/cognitive testing and a blood draw before and after completing one of the interventions.
Data Release
- The first data release includes 20 unique subjects.
- The second data release includes 110 unique subjects, 90 with repeat data.
- The third data release includes 110 unique subjects, 90 with repeat data.
- Gene expression raw and analyzed data will be deposited in the Gene Expression Omnibus (GEO) database ( http://www.ncbi.nlm.nih.gov/geo) at the end of the project.
Keywords
Major Depression, Mood Disorders, White Matter, Functional Connectivity, Structural Connectivity, Neuroplasticity, Antidepressant
Current Data Releases
PDC 1.0 Release Released on 04/27/2023
PDC Release 1.0 of imaging and behavioral data is now available in the NIMH Data Archive (NDA). Perturbation of the depression connectome by fast-acting therapies (Perturbation of the Depression Connectome, PDC) is a study of adults with and without treatment resistant depression (191 patients, 51 controls) and with and without fast-acting treatment interventions (ages 20-64, with treatment-resistant depression treated with ECT [N=44], ketamine [N=67], or total sleep deprivation [N=60], plus healthy controls [N=51]). Of the healthy controls, 16 underwent total sleep deprivation and 17 were assessed at 2 visits without intervention.
PDC Release 1.0 data includes:
- unprocessed data of all modalities (structural MRI, resting state fMRI, task fMRI for 2 tasks, and diffusion MRI) for 227 subjects
- minimally preprocessed MRI data of all modalities for up to 218 subjects
- clinical and behavioral data for 230 subjects
Get Access and Download the data: Get started with the Data Access and Download Instructions for obtaining access, navigating NDA and using it's download tools. We've also created a wiki that details setup steps for downloading data via NDA's command line tools.
The released data are available on NDA as:
- PDCRec package of recommended preprocessed + behavioral data (1076 GB, OPTION ONE)
- PDCAllFiles package of all released imaging and behavioral data (9.5 TB, OPTION ONE)
- PDCImgManifestBeh package of imaging manifests + behavioral data (332 MB, OPTION ONE)
- or can be filtered on to create a custom package of a subset of the data (OPTION TWO).
Want more information? Check out our documentation to help with understanding the project and interpreting the data.
View Data Release Documentation
Release Date: Apr 27, 2023
Publications
-
Modulation of intrinsic brain activity by electroconvulsive therapy in major depression.
Show SummaryOne of the most effective interventions for intractable major depressive episodes is electroconvulsive therapy (ECT). Because ECT is also relatively fast-acting, longitudinal study of its neurobiological effects offers critical insight into the mechanisms underlying depression and antidepressant response. Here we assessed modulation of intrinsic brain activity in corticolimbic networks associated with ECT and clinical response.
-
Structural connectivity and response to ketamine therapy in major depression: A preliminary study.
Show SummaryKetamine elicits an acute antidepressant effect in patients with major depressive disorder (MDD). Here, we used diffusion imaging to explore whether regional differences in white matter microstructure prior to treatment may predict clinical response 24h following ketamine infusion in 10 MDD patients.
-
Desynchronization and Plasticity of Striato-frontal Connectivity in Major Depressive Disorder.
Show SummaryMajor depressive disorder (MDD) is associated with dysfunctional corticolimbic networks, making functional connectivity studies integral for understanding the mechanisms underlying MDD pathophysiology and treatment. Resting-state functional connectivity (RSFC) studies analyze patterns of temporally coherent intrinsic brain activity in "resting-state networks" (RSNs). The default-mode network (DMN) has been of particular interest to depression research; however, a single RSN is unlikely to capture MDD pathophysiology in its entirety, and the DMN itself can be characterized by multiple RSNs. This, coupled with conflicting previous results, underscores the need for further research. Here, we measured RSFC in MDD by targeting RSNs overlapping with corticolimbic regions and further determined whether altered patterns of RSFC were restored with electroconvulsive therapy (ECT). MDD patients exhibited hyperconnectivity between ventral striatum (VS) and the ventral default-mode network (vDMN), while simultaneously demonstrating hypoconnectivity with the anterior DMN (aDMN). ECT influenced this pattern: VS-vDMN hyperconnectivity was significantly reduced while VS-aDMN hypoconnectivity only modestly improved. RSFC between the salience RSN and dorsomedial prefrontal cortex was also reduced in MDD, but was not affected by ECT. Taken together, our results support a model of ventral/dorsal imbalance in MDD and further suggest that the VS is a key structure contributing to this desynchronization.
-
Electroconvulsive therapy mediates neuroplasticity of white matter microstructure in major depression.
Show SummaryWhether plasticity of white matter (WM) microstructure relates to therapeutic response in major depressive disorder (MDD) remains uncertain. We examined diffusion tensor imaging (DTI) correlates of WM structural connectivity in patients receiving electroconvulsive therapy (ECT), a rapidly acting treatment for severe MDD. Tract-Based Spatial Statistics (TBSS) applied to DTI data (61 directions, 2.5 mm(3) voxel size) targeted voxel-level changes in fractional anisotropy (FA), and radial (RD), axial (AD) and mean diffusivity (MD) in major WM pathways in MDD patients (n=20, mean age: 41.15 years, 10.32 s.d.) scanned before ECT, after their second ECT and at transition to maintenance therapy. Comparisons made at baseline with demographically similar controls (n=28, mean age: 39.42 years, 12.20 s.d.) established effects of diagnosis. Controls were imaged twice to estimate scanning-related variance. Patients showed significant increases of FA in dorsal fronto-limbic circuits encompassing the anterior cingulum, forceps minor and left superior longitudinal fasciculus between baseline and transition to maintenance therapy (P<0.05, corrected). Decreases in RD and MD were observed in overlapping regions and the anterior thalamic radiation (P<0.05, corrected). Changes in DTI metrics associated with therapeutic response in tracts showing significant ECT effects differed between patients and controls. All measures remained stable across time in controls. Altered WM microstructure in pathways connecting frontal and limbic areas occur in MDD, are modulated by ECT and relate to therapeutic response. Increased FA together with decreased MD and RD, which trend towards normative values with treatment, suggest increased fiber integrity in dorsal fronto-limbic pathways involved in mood regulation.
Data Use Terms
When users request access to the NIMH Data Archive (NDA), they sign the NDA Data Use Certification (DUC) under which the data is shared. This DUC is usually submitted to the NDA electronically, but this printable version can also be submitted to NDAhelp@mail.nih.gov.
More information on obtaining NDA access is available in the Data Access and Download Instructions.